Poop Bacteria versus C. difficile: Pathogen Proves to be a Complex Opponent in the Battle Between Good and Bad Gut Bacteria
By Madison Wright
29 May 2019
In 2011, the Guelph General Hospital was the site of a significant Clostridioides difficile outbreak, a potentially fatal bacterial infection that causes diarrhea, fever and severe pain. The outbreak left many Guelphites wondering what makes the bug so deadly and why the number of C. difficile infections at Guelph General seemed to be growing.
Prof. Emma Allen-Vercoe, a microbiologist in the Department of Molecular and Cellular Biology, was also curious about the pathology of C. difficile. She knew the scientific literature hinted at a potential connection between C. difficile infections and a lack of healthy gut bacteria. At the time, scientific interest in the gut “microbiome” was just beginning to take off, and Allen-Vercoe – a world expert in culturing gut microbes – decided to delve into the potential link to C. difficile.
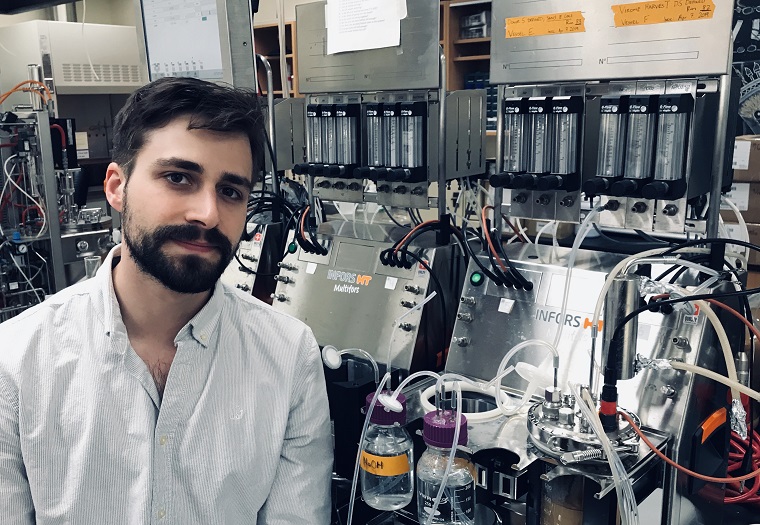
Working closely with Allen-Vercoe was Christian Carlucci who started a summer job during his undergraduate degree in the Allen-Vercoe lab, which eventually led to a PhD. Today, Carlucci can still be found working closely with Allen-Vercoe as a research scientist at NuBiyota, a spin-off company co-founded by Allen-Vercoe. The company is working to commercialize microbial therapeutics to treat C. difficile – showing just how far the science has come since that 2011 outbreak in Guelph.
Carlucci and Allen-Vercoe recently published a major study based on Carlucci’s PhD research that gives new insights into the complexity of this troublesome pathogen, particularly when it comes to treating it with “healthy” gut bacteria.
The study saw Carlucci carry out an investigation of the effect of the chemical compounds produced by healthy gut bacteria on C. difficile, wanting to know if these compounds alone would be sufficient to reduce the infectious capabilities of C. difficile. First, he cultured different groups of “good” bacteria from the stool of a healthy donor. One of these groups was treated with antibiotics to mimic the situation where a patient’s good gut microbes are weakened by antibiotics, leaving them at a higher risk of C. difficile infection. Carlucci then removed the bacterial cells, leaving only the chemical compounds produced by the bacteria.
Carlucci and his colleagues then treated C. difficile with the compounds and assessed the growth of the pathogen, toxin production, and its ability to form spores (which allows the bug to survive harsh conditions). Knowing the pathogen can be highly complex, Carlucci tested the compounds on two distinct strains of C. difficile. The first, known as CD186, is a highly infectious and transmissible strain found in hospitals that produces multiple toxins. The second strain, CD973, is a less troublesome version that is more commonly found in the community.
The researchers were surprised to find that when it comes to combatting bad bugs with good bugs, not all pathogen strains behave equally.
"We found that the products from the ‘good’ bacteria influenced the two C. difficile strains differently,” says Carlucci.
The findings may explain why it can be difficult to treat infections with microbial-based therapeutics. For example, when the highly infectious strain (CD186) was treated with the products from the bacteria exposed to antibiotics, it led to increased toxin production. This reinforces the idea that antibiotic treatment can indirectly increase C. difficile’s infectious capabilities, resulting in a more serious problem for patients.
Currently, fecal transplants are used to treat C. difficile infections when antibiotics fail. Fecal transplants involve the transfer of stool from a healthy person to the gut of an infected person, with the goal of increasing the army of resident good bacteria and, ideally, enabling them to outcompete this nasty pathogen.
This strategy has shown great promise in treating C. difficile, but it’s far from a silver bullet.
“Healthcare regulations are moving away from fecal transplants as it is hard to ensure adequate safety and consistency,” explains Carlucci. “This is because the stool comes from different donors and is collected at different times, potentially leading to different treatment results.”
This is what’s driving efforts at NuBiyota, where the focus is on developing a standardized microbial treatment that has been cultured in the laboratory, instead of relying on human donors. Fittingly, Carlucci’s PhD research is helping the company figure out the optimal microbiome therapeutic to move forward with in clinical tests.
“The most exciting part of this research is that it is relevant,” says Carlucci. “We are talking about a problem that still affects people. With better antimicrobial stewardship in hospitals we have fewer C. difficile cases, but there are still patients suffering with complex infections. Not everyone gets better after antibiotics, or even multiple courses of antibiotics. This work is exploring a therapy that has a huge potential to save a lot of lives in the near future.”
This study was funded by the National Institute of Health and the Physicians’ Services Incorporated Grant in Aid of Research.
Read the full study in the journal Scientific Reports.
Read about other CBS Research Highlights.